Achilles Tendon Rupture How Do I Know I Have Got It?
Overview 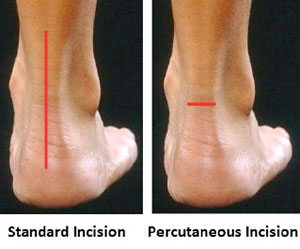 An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears). Causes The causes of an Achilles tendon rupture are very similar to Achilles tendinitis. Causes include. Running uphill. Running on a hard surface. Quickly changing speeds from walking to running. Playing sports that cause you to quickly start and stop. Symptoms Patients who suffer an acute rupture of the Achilles tendon often report hearing a ?pop?or ?snap.? Patients usually have severe pain the back of the lower leg near the heel. This may or may not be accompanied by swelling. Additionally, because the function of the Achilles tendon is to enable plantarflexion (bending the foot downward), patients often have difficulty walking or standing up on their toes. With a complete rupture of the tendon, the foot will not move. In cases where the diagnosis is equivocal, your physician may order an MRI of the leg to diagnose a rupture of the Achilles tendon. Diagnosis In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes. The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests. Non Surgical Treatment Non-surgical treatment of Achilles tendon rupture is usually reserved for patients who are relatively sedentary or may be at higher risk for complications with surgical intervention (due to other associated medical problems). This involves a period of immobilization, followed by range of motion and strengthening exercises; unfortunately, it is associated with a higher risk of re-rupture of the tendon, and possibly a less optimal functional outcome.
An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears). Causes The causes of an Achilles tendon rupture are very similar to Achilles tendinitis. Causes include. Running uphill. Running on a hard surface. Quickly changing speeds from walking to running. Playing sports that cause you to quickly start and stop. Symptoms Patients who suffer an acute rupture of the Achilles tendon often report hearing a ?pop?or ?snap.? Patients usually have severe pain the back of the lower leg near the heel. This may or may not be accompanied by swelling. Additionally, because the function of the Achilles tendon is to enable plantarflexion (bending the foot downward), patients often have difficulty walking or standing up on their toes. With a complete rupture of the tendon, the foot will not move. In cases where the diagnosis is equivocal, your physician may order an MRI of the leg to diagnose a rupture of the Achilles tendon. Diagnosis In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes. The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests. Non Surgical Treatment Non-surgical treatment of Achilles tendon rupture is usually reserved for patients who are relatively sedentary or may be at higher risk for complications with surgical intervention (due to other associated medical problems). This involves a period of immobilization, followed by range of motion and strengthening exercises; unfortunately, it is associated with a higher risk of re-rupture of the tendon, and possibly a less optimal functional outcome.  Surgical Treatment This injury is often treated surgically. Surgical care adds the risks of surgery, there are for you to view. After the surgery, the cast and aftercare is typically as follows. A below-knee cast (from just below the knee to the tips of the toes) is applied. The initial cast may be applied with your foot positioned in a downward direction to allow the ends of the tendon to lie closer together for initial healing. You may be brought back in 2-3 week intervals until the foot can be positioned at 90 degrees to the leg in the cast. The first 6 weeks in the cast are typically non-weight bearing with crutches or other suitable device to assist with the non-weight bearing requirement. After 6 weeks in the non-removable cast, a removable walking cast is started. The removable walking cast can be removed for therapy, sleeping and bathing. The period in the removable walking cast may need to last for an additional 2-6 weeks. Your doctor will review a home physical therapy program with you (more on this program later) that will typically start not long after your non-removable cast is removed. Your doctor may also refer you for formal physical therapy appointments. Typically, weight bearing exercise activities are kept restricted for at least 4 months or more. Swimming or stationary cycling activities may be allowed sooner. Complete healing may take 12 months or more.
Surgical Treatment This injury is often treated surgically. Surgical care adds the risks of surgery, there are for you to view. After the surgery, the cast and aftercare is typically as follows. A below-knee cast (from just below the knee to the tips of the toes) is applied. The initial cast may be applied with your foot positioned in a downward direction to allow the ends of the tendon to lie closer together for initial healing. You may be brought back in 2-3 week intervals until the foot can be positioned at 90 degrees to the leg in the cast. The first 6 weeks in the cast are typically non-weight bearing with crutches or other suitable device to assist with the non-weight bearing requirement. After 6 weeks in the non-removable cast, a removable walking cast is started. The removable walking cast can be removed for therapy, sleeping and bathing. The period in the removable walking cast may need to last for an additional 2-6 weeks. Your doctor will review a home physical therapy program with you (more on this program later) that will typically start not long after your non-removable cast is removed. Your doctor may also refer you for formal physical therapy appointments. Typically, weight bearing exercise activities are kept restricted for at least 4 months or more. Swimming or stationary cycling activities may be allowed sooner. Complete healing may take 12 months or more.